COVID-19 was making its way through Central Florida in early March, back when hospitals were not fully prepared to identify the symptoms, which can appear similar to the flu, and didn’t have easy access to get quick test results.
Joan Steinhauer went on a family cruise to the Bahamas Feb. 10 and returned on the 14th. About three weeks later, she started to run a fever.
“She was running a low-grade fever, nothing to be excited about, it was like 99.4, this was the first part of March,” her daughter, Ann Day, told Channel 9 investigative reporter Daralene Jones.
READ: Florida governor says phase 1 of reopening can begin May 4, except in 3 South Florida counties
The next day, on March 9, her temperature jumped to 103.5, and that’s when Day knew she had to get her mother to Dr. Phillips Hospital in Orlando.
“They admitted her, took a bunch of tests, they all came back negative,” Day said. “They did a strep test, flu test, chest X-ray for pneumonia. They thought maybe she had a false negative on her flu, sent her home with Tamiflu and a Z-pack and I brought her to my house to take care of her.”
Day said the antibiotics did not seem to work. In fact, her 79-year-old mother only got worse, so she took her back to the same emergency room.
“The Z-pack, the Tamiflu, I couldn't keep it in her system. And she just got so bad,” Day said. “They went ahead and ran the same tests again. Everything came back negative again.”
She gave Orlando Health permission to discuss her mother’s case with 9 Investigates. A spokesperson who consulted with the doctor who treated Steinhauer said she developed difficulty breathing and low oxygen level on March 13.
READ: Coronavirus: Denied unemployment benefits in Florida? Here’s what you need to do
A spokesperson told us they took cultures from Steinhauer then, which could be used to test for COVID-19, but at that point the tests were going to one distant lab that turned around and sent it to another.
Orlando Health did not get that result until March 21, a delay which hospitals were experiencing across the country because it was the first week of commercial testing. Until that point everything was going to the Department of Health.
The doctor said Steinhauer was given tocilizumab, which is a medicine to control the inflammatory response and they also started an antiviral, lopinavir-ritonavir, because they wanted to see if they could obtain remdesivir, an anti-viral medication, once the diagnosis was confirmed.
Steinhauer deteriorated the day after hospital officials took the cultures. The doctor said he contacted a local lab to see if they could help, and the results were processed overnight. The result came on the morning of March 15. And hospital officials said that was the same day of Steinhauer’s death.
It wasn’t until 10 days after her death that the state health department opened the first public testing site in Central Florida at the Orange County Convention Center.
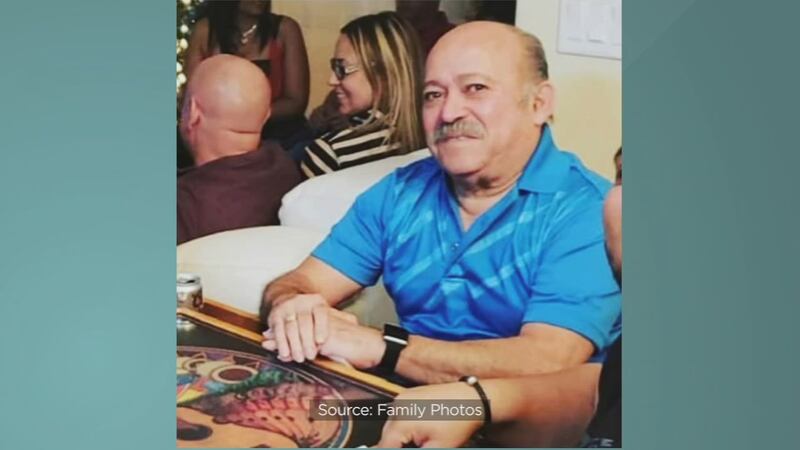
Days later, 81-year-old Jules Greene was admitted to Health Central because of chills, cough and diarrhea, his wife confirmed to Jones over the telephone this week.
Greene’s medical examiner’s report shows he was placed on a BiPAP breathing machine in the critical care unit but continued to decline. Two days into his stay he was tested, and it came back positive.
Greene’s widow told us hospital officials told her then that she didn’t need to be tested, but should stay in self-isolation. Meanwhile, she was kept away from her spouse of several days while he was intubated and placed on a ventilator.
Mayor Jerry Demings got emotional speaking about Greene during a news conference in early April. After that day she told me over the phone she was tested and it came back positive, but she never had any symptoms.
Steinhauer died the day before her test came back positive. By then, because she had been in and out of the hospital in a weeks' time, she had infected three other family members, including her daughter Ann, who made a personal decision after her recovery to donate her plasma for convalescent plasma therapy underway at Orlando Health.
Doctors believe it's already helped other patients fight off the virus.
The process is complicated as donors' blood types must be compatible with recipients. And donors must be symptom free for at least 14 days and FDA approval is required.
“It’s heart-wrenching,” Day said. “I know she would be just so devastated to know what has happened in the family and that she was any part of that, but she would be very happy with the fact that I’ve picked up and moved on. I’m proud of myself.”
© 2020 Cox Media Group